Lungs
Partial pressure
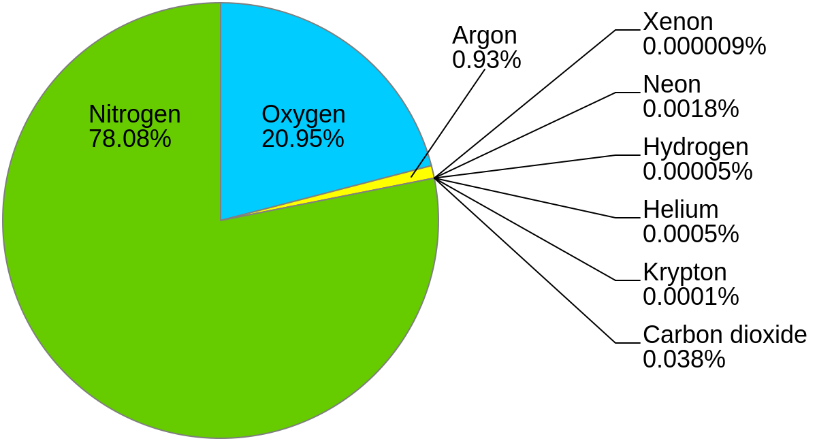
Air is composed out of couple of gases, the major part take nitrogen, oxygen and argon (for simplification, we will ignore the others). Properties, that are generally being changed for every gas mixture are pressure (P), volume (V) an temperature (T). When changing one parameter, the other two change also, according to equation: $$ {P_1×V_1 \over T_1} ={P_2×V_2 \over T_2}$$ The value that always stays the same, is absolute amount of gas, expressed in number of molecules (if we do not add or take away from the mixture). That is explained by gas equation, where n represents the number of molecules: $$ P×V=n×R×T$$ Now imagine this scenario: we take a tank with constant volume and constant temperature, so we get equation: $$ P=n×R $$ If we want a higher pressure, we can only add more gas, or, if we take it away, the pressure will drop, both in linear fashion. According to that, the pressure is intrinsic property of every amount of gas; bigger the amount, bigger the pressure is.
mmHg
21% of mmHg = mmHg
Other gasses:
79% of mmHg = mmHg
So, if we take again the air mixture, and compare nitrogen (78%) and oxygen (21%) at pressure 1 atm, we can conclude, that pressure contributed by nitrogen is 78% of 1 atm (0,78 atm) and the pressure contributed by oxygen is 21% of 1 atm (0,21 atm). Pressure, contributed to the mixture according to the part, the gas itself takes, is called a partial pressure. $$P_x=F_x×P_{BAR}$$
In real life, what most commonly affect the value of pressure, is climbing to higher altitudes or going under water. When we go higher, the layer of air above us gets thinner, that why the pressure drops; the opposite happens when we decline. When we go under water, the pressure changes with depth more dramatically, because of much higher water density. The air pressure at the sea level is around 760 mmHg; at the highest point on earth, Mt. Everest, the pressure drops to only 243 mmHg! So if we consider that percentage of oxygen stays the same at all altitudes (21%), we can calculate that partial pressure of oxygen at sea level is around 160 mmHg, but at the summit of the highest mountain in the world is only 51 mmHg.
Factor, that most commonly affects the change in atmospheric pressure and therefore partial pressure of oxygen in real life, is change in altitude. If we take in consideration only places, accessible on foot, we get a range from 0m to 8848m off the sea level (the hight of Mount Everest). Moving between these altitudes, atmospheric pressure changes from 760 mmHg at the se level to 422 mmHg at the summit of Mount Everest.
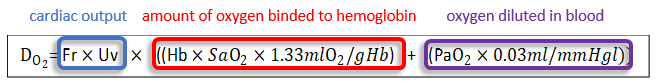
BOUND AND FREELY DISSOLVED OXIGEN
In blood, oxygen is carried in two forms: bound to haemoglobin and freely dissolved. Amount of oxygen, bound to the haemoglobin, is described with haemoglobin dissociation curve; on the x axis we have partial pressure and on the y axis percentage of saturated haemoglobin. Higher the partial pressure of oxygen, better the saturation of haemoglobin. Total amount of oxygen, brought around the body on haemoglobin, can by therefore expressed by multiplying cardiac output (L/min), amount of oxygen that can be carried by one gram of haemoglobin (mLO2/gHb), concentration of haemoglobin (gHb/L) and percentage of saturation. Amount of oxygen, freely dissolved in blood, is described by Henry's law; $$[gas]_{diluted}=P_{gas}×s$$ It depends on partial pressure of gas (mmHg) and it's solubility (0,03ml/mmHg). If we want to calculate whole amount of oxygen, carried by blood in one minute, we can calculate it by this equation:
Bohr effect
The Bohr effect describes haemoglobin’s variability in affinity for oxygen secondary to change in the partial
pressure of carbon dioxide and blood pH (higher the PCO2, lower the pH). The change in H+ affects the
proteins of haemoglobin, which is visible in different capacity or oxygen affinity, if you want, at different
partial pressure of oxygen.
At higher PCO2 and therefore lower pH, the haemoglobin curve shifts right.
At lower PCO2
and therefore higher pH, the haemoglobin curve shifts left.
Lower affinity at high CO2 partial
pressure and lower pH enhances the unloading of oxygen into tissues to meet the oxygen demand of the tissue.
Beside PCO2 and therefore pH, there are also DPG (diphosphoglycerate, which is made in process of
glycolysis) and temperature which affect haemoglobin affinity for oxygen. In higher metabolic rates, both DPG
and body temperature increase, leading to right shift of haemoglobin dissociation curve and the opposite occurs
in lower values of DPG and body temperature. So, if we look at the whole picture; at higher physical activity,
PCO2, DPG, and body temperature will rise, and the pH will fall. All of this will lead to the right
shift of haemoglobin dissociation curve. In lower physical activity, PCO2, DPG and body temperature
will fall and the pH will rise. All of this will lead to the left shift of haemoglobin dissociation curve.
Haldane effect
Haldane effect states that oxygenation of blood causes higher dissociation of carbon dioxide from haemoglobin and vice versa. This effect is very important for better excretion of excess CO2 from the body; without it, the average amount of CO2, remaining in the body, would be higher. In lungs, where partial pressure of oxygen rises, more CO2 will dissociate from haemoglobin and leave the body with exhaled air, but in the periphery, where partial pressure of oxygen is lower, more CO2 will bind to haemoglobin and leave the tissue.
Partial pressures along respiratory tract
$$ {P_1×V_1 \over T_1} ={P_2×V_2 \over T_2}$$
Column 1
It represents the partial pressure of oxygen in the air. It depends on percentage of oxygen and atmospheric
pressure. $$ {P_{IO2}=F_{O2}×P_{BAR}}$$Column 2
It describes intratracheal partial pressure of
oxygen. The reason, why it gets lower, is humidification of air, so the partial pressure of water takes it`s
part of atmospheric pressure (47 mmHg). $${P_{ITO2}=F_{O2}×(P_{BAR}−P_{H2O})}$$ $${P_{ITO2}=F_{O2}×(P_{BAR}−47
mmHg)}$$Column 3
It represents the partial pressure of oxygen in alveoli. It depends on intratracheal partial pressure of oxygen,
consumption of oxigen, atmospheric pressure and alveolar ventilation. $${P_{AO2}=P_{ITO2}−{V_{O2}×P_{BAR} \over
AV}×k }$$ Column 4
It represents the partial pressure of oxygen in arterial blood. Theoretically, partial pressure of oxygen in
arterial blood and alveoli should level out when reaching the equalibrium, but in reallity this is very hard to
achieve. There is always some level of shunt, alveolar ventilation/perfusin mismach, defect in diffusion of
oxygen from alveoli into the blood… so the value of partial pressure of oxygen in arterial blood is slightly
lower (in this graph, we persume that partial pressures of oxygen in arterial blood and alveoli level out
perfectly).
Column 5
It describes the partial pressure of oxygen in venous blood,
returning to the lungs. To calculate the right value of it, you have to know 1) the arterial partial pressure of
oxygen, 2) consumption of oxygen and you need to have 3) the exact haemoglobin dissociation curve for that
state, so you can make the readings. In first step, you check what is the percentage of saturation of
haemoglobin in arterial blood. From saturation value, you can calculate the amount of oxygen, that is bound to
haemoglobin (at 100% of saturation, there is approximately 200 mL of oxygen per litre of blood). From that
value, you take away the amount of oxygen that is being used every minute per litre of blood, and what you get,
is amount of oxygen in one litre of venous blood. From this, you go into the opposite direction; you calculate
what is the saturation of haemoglobin and for that saturation value, you read the partial pressure of oxygen in
venous blood from the haemoglobin dissociation curve. This is the value, presented by column five.
